New patch aims to turn energy-storing fats into energy-burning fats
 A new approach to reducing bulging tummy fats has shown promise in laboratory trials. It combines a new way to deliver drugs, via a micro-needle patch, with drugs that are known to turn energy-storing white fat into energy-burning brown fat. This innovative approach developed by scientists from Nanyang Technological University, Singapore (NTU Singapore) reduced weight gain in mice on a high fat diet and their fat mass by more than 30 per cent over four weeks. This is good news for fat mice, but fat humans will need to wait until human trials start.
A new approach to reducing bulging tummy fats has shown promise in laboratory trials. It combines a new way to deliver drugs, via a micro-needle patch, with drugs that are known to turn energy-storing white fat into energy-burning brown fat. This innovative approach developed by scientists from Nanyang Technological University, Singapore (NTU Singapore) reduced weight gain in mice on a high fat diet and their fat mass by more than 30 per cent over four weeks. This is good news for fat mice, but fat humans will need to wait until human trials start.
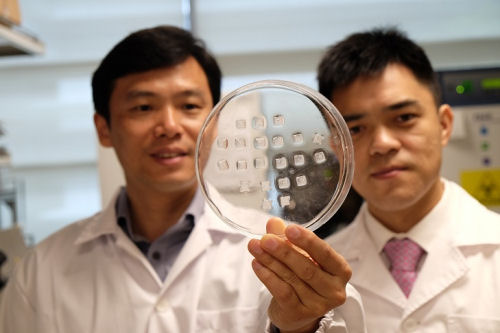
NR Banner - Prof Chen Peng (left) holding the drug-laden microneedle fat burning patch with Asst Prof Xu Chenjie - Copy.JPG
A new approach to reducing bulging tummy fats has shown promise in laboratory trials.
This article reports on the following scientific report: Aung Than, Ke Liang, Shaohai Xu, Lei Sun, Hongwei Duan, Fengna Xi, Chenjie Xu, Peng Chen. Transdermal Delivery of Anti-Obesity Compounds to Subcutaneous Adipose Tissue with Polymeric Microneedle Patches. Small Methods, 2017; 1 (11): 1700269 DOI: 10.1002/smtd.201700269 to be found at https://onlinelibrary.wiley.com/doi/10.1002/smtd.201700269/abstract.
"Excess white adipose tissue (WAT), or obesity, is the leading cause of many diseases. Combating obesity is, however, challenging due to the fact that laboratory-proven anti-obesity compounds lose effectiveness or/and cause severe side-effects while being delivered via conventional routes. Here, a new strategy is reported using disposable transdermal patches equipped with detachable polymeric microneedle (MN) arrays for painless and bloodless drug delivery to subcutaneous WAT. In contrast to the current methods to reduce energy intake, MN-patches are used to deliver anti-obesity compounds to increase energy expenditure by transforming calorie-storing white fat into calorie-burning brown fat. Specifically, prominent WAT browning and reduction effects are demonstrated by β3-adrenoceptor agonist and thyroid hormone T3 transdermally delivered from rapidly dissolving MNs on mice. Furthermore, using a diet-induced obese mouse model, it is shown that β3-adrenoceptor agonist released by slowly dissolving MNs can effectively promote WAT browning and suppress gaining of body fat and weight, without the need of daily administration. Such an MN approach can achieve a much lower effective dose as compared to systemic administration and enables long-term home-based treatment."
The new type of skin patch contains hundreds of micro-needles, each thinner than a human hair, which are loaded with the drug Beta-3 adrenergic receptor agonist or another drug called thyroid hormone T3 triiodothyronine.
When the patch is pressed into the skin for about two minutes, these micro-needles become embedded in the skin and detach from the patch, which can then be removed.
As the needles degrade, the drug molecules then slowly diffuse to the energy-storing white fat underneath the skin layer, turning them into energy-burning brown fats.
Brown fats are found in babies and they help to keep the baby warm by burning energy. As humans grow older, the amount of brown fats lessens and is replaced with visceral white fats.
Published in the journal Small Methods recently by NTU Professor Chen Peng and Assistant Professor Xu Chenjie, this approach could help to address the worldwide obesity problem without resorting to surgical operations or oral medication which could require large dosages and could have serious side effects.
“With the embedded microneedles in the skin of the mice, the surrounding fats started browning in five days, which helped to increase the energy expenditure of the mice, leading to a reduction in body fat gain,” said Asst Prof Xu, who focuses on research in drug delivery systems.
“The amount of drugs we used in the patch is much less than those used in oral medication or an injected dose. This lowers the drug ingredient costs while our slow-release design minimises its side effects,” said Asst Prof Xu.
Obesity which results from an excessive accumulation of fat is a major health risk factor for various diseases, including heart disease, stroke and type-2 diabetes. The World Health Organisation estimates that 1.9 billion adults in the world are overweight in 2016 with 650 million of them being obese.
“What we aim to develop is a painless patch that everyone could use easily, is unobtrusive and yet affordable,” said Prof Chen, a biotechnology expert who researches on obesity. “Most importantly, our solution aims to use a person’s own body fats to burn more energy, which is a natural process in babies.”
Under the two scientists’ guidance at NTU’s School of Chemical and Biomedical Engineering, research fellow Dr Aung Than conducted experiments which showed that the patch could suppress weight gain in mice that were fed a high fat diet and reduce their fat mass by over 30 per cent, over a period of four weeks.
The treated mice also had significantly lower blood cholesterol and fatty acids levels compared to the untreated mice.
Being able to deliver the drug directly to the site of action is a major reason why it is less likely to have side effects than orally delivered medication.
The team estimates that their prototype patch had a material cost of about S$5 (US$3.50) to make, which contains beta-3 adrenergic receptor agonist combined with Hyaluronic acid, a substance naturally found in the human body and commonly used in products like skin moisturisers.
Beta-3 adrenergic receptor agonist is a drug approved by the Federal Drug Administration of the United States and is used to treat overactive bladders, while T3 triiodothyronine is a thyroid hormone commonly used for medication for an underactive thyroid gland.
Both have been shown in other research studies to be able to turn white fats brown, but their use in reducing weight gain is hampered by potentially serious side-effects and drug accumulation in non-targeted tissues if conventional drug delivery routes were used, such as through oral intake.
NTU’s Lee Kong Chian School of Medicine Associate Professor Melvin Leow, who was not affiliated with this study, said it is exciting to be able to tackle obesity via the browning of white fat, and the results were promising.
“These data should encourage Phase I Clinical studies in humans to translate these basic science findings to the bedside, with the hope that these microneedle patches may be developed into an established cost-effective modality for the prevention or treatment of obesity in the near future,” added Assoc Prof Leow, an endocrinologist.
Since the publication of the paper, the team has received keen interest from biotechnology companies and is looking to partner clinician scientists to further their research.
Source: From a press release dated
Published on: 28-Dec-2017 and issued by Nanyang Technological University, Singapore.

Recent comments