 What gives with surveys that tell us that most of us want more immigrants and a bigger population when, all around us, we suffer the effects of faster and faster population growth in groaning infrastructure, costly housing, road congestion, and rising costs for power and water? If we examine such studies, we will find that they pose their questions in the abstract and do not prompt people to make concrete associations about the effects of immigration and population growth. This is a bit like asking people how they feel about war compared to asking how they feel about war in their suburb. These polls also focus on ethnicity of immigrants rather than environment and planning impacts of mass migration. This article looks at recent polls by the Australian Institute of Progress, Roy Morgan Research, the Australian Election Study and Queensland Growth Management Summit 2010, Social Research on Population Growth and Liveability in South East Queensland". The Queensland survey is the most detailed and valid and has been discussed in its own article, "Poll shows most hate population growth: Lessons from Queensland in polling reliability and interpretation."
What gives with surveys that tell us that most of us want more immigrants and a bigger population when, all around us, we suffer the effects of faster and faster population growth in groaning infrastructure, costly housing, road congestion, and rising costs for power and water? If we examine such studies, we will find that they pose their questions in the abstract and do not prompt people to make concrete associations about the effects of immigration and population growth. This is a bit like asking people how they feel about war compared to asking how they feel about war in their suburb. These polls also focus on ethnicity of immigrants rather than environment and planning impacts of mass migration. This article looks at recent polls by the Australian Institute of Progress, Roy Morgan Research, the Australian Election Study and Queensland Growth Management Summit 2010, Social Research on Population Growth and Liveability in South East Queensland". The Queensland survey is the most detailed and valid and has been discussed in its own article, "Poll shows most hate population growth: Lessons from Queensland in polling reliability and interpretation."
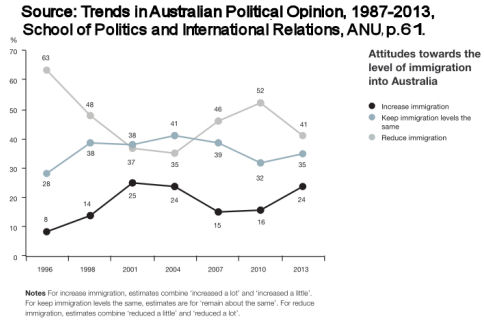
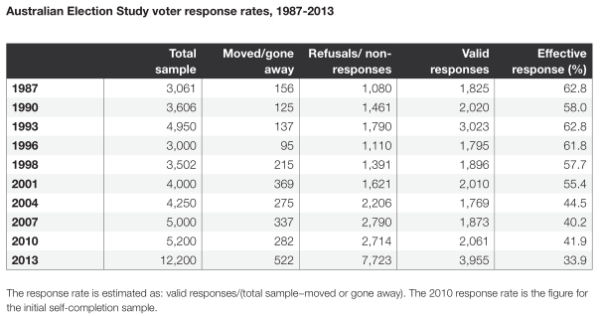
In 2013 the Australian Election Study found that only 24% of Australians supported higher levels of immigration. It received 3,955 valid responses from an initial sample of 12,200 people. The survey is conducted on paper via snail-mail or online. There are prizes to motivate timely responses. [1] This survey is known as Australia's biggest and most reliable, but, as the table below shows, its response rate has been falling every year.
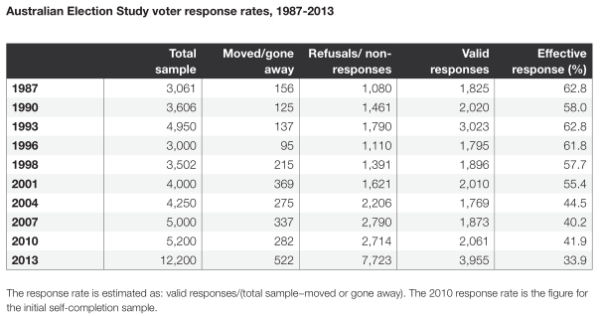
Responses to telephone polls, however, are an order of magnitude dimmer, at 9-17%. This is the method that the Roy Morgan institute uses. The Australian Institute of Progress uses on-line surveys of a particular population it has gathered over the years, but that population cannot be said to represent the average Australian's point of view.
On October 15, 2015 the Australian Institute of Progress (AIP)came out with [usable] poll results from 1349 people which it claimed showed that 69% of those polled supported higher immigration. The poll received inordinate publicity from a mass media eager to promote rapid population growth in Australia, [2] with The Australian interpreting the result to mean that "69 per cent of Australians support high rates of immigration."
On October 20, 2015, Roy Morgan also came out with poll results from 650 people: A majority of Australians support higher immigration and an Australian population over 30 million. This predictably also received huge publicity in the mass media.
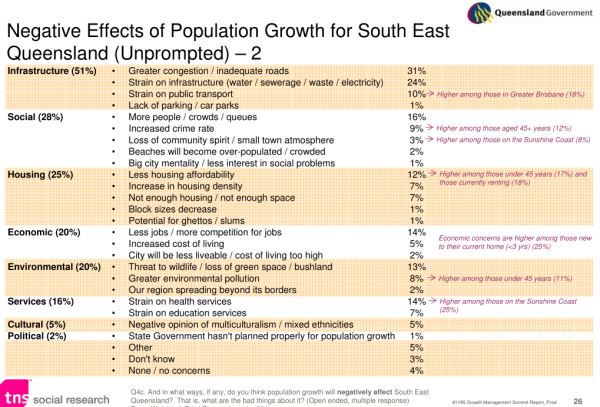
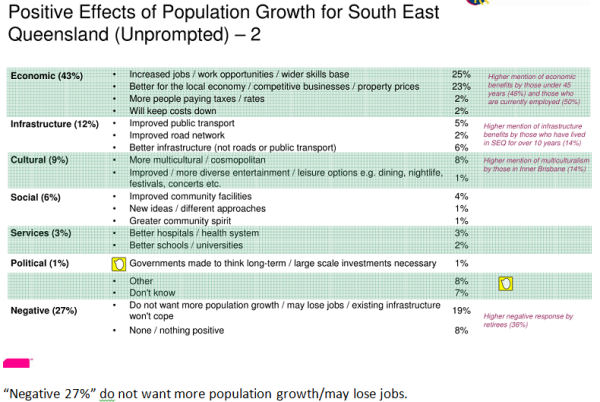
Claims that most Australians suddenly support higher immigration [3] and an Australian population of over 30 million are hard to take on face value, especially in the light of the results of the Queensland survey: "Queensland Growth Management Summit 2010, Social Research on Population Growth and Liveability in South East Queensland", March 2010 [4], a probed survey with 801 respondents which showed that about 90% experienced population growth as having a negative impact on their lives. My experience between 1994 and 2015 (the period I have been studying attitudes to population growth) is that more and more people are speaking out against the many effects of high immigration and rapid population growth. That's not surprising, since the effects have been more and more noticeable as the population has grown more and more rapidly.
So I took a look at the questions, the numbers and the method in the AIP and the Roy Morgan polls.
Why would most Australians tick a box for a population over 30 m but less than 35m in the Roy Morgan poll?
"A majority of Australians support higher immigration and an Australian population over 30 million."
I find it interesting that the respondents in this poll apparently endorsed 'under 35 million' but did not endorse '35 million or more', and did not choose 'Under 30 million'. How did they make such a distinct choice? How were the population number choices proposed?
This is how the Roy Morgan poll posed the question of population size:
“Australia’s population has increased by 6 million from 18 million to 24 million over the last 20 years. What population do you think we should aim to have in Australia in 30 years – that is, by 2045?”
Under 25 million 9%
25 - Under 30 million 23%
30 – Under 35 million 27%
35 – Under 40 million 16%
40 – Under 50 million 10%
50 million or more 4%
Can’t say 11%
There are a number of things I find odd about these responses and the interpretations made.
Why, for instance, did more people not select the last three options, if they want a bigger population? The choice of 30m or no more than 35m does not signal enthusiasm for a big population; rather a desire to remain at the lower end of the scale they were presented with as the choices. How, I wonder, did they make these choices? Were they under the impression that what they were selecting was either mathematically reasonable or appeared more 'generous'? Or, given the historic growth described as going from 18 m to 24m in 20 years, did they assume some arithmetical trend of six million every 20 years, and therefore a sequence of 18:24:30? Which would mean that they stopped at the lowest possible logical number sequence?
My own experience of talking to people about population numbers, including conducting polls at the Sustainable Living Festival, is that many have only the faintest idea of what Australia's population is now, or the world's. They seem to be unable to quantify or imagine these numbers. 24m might mean little to them. The rates of population growth that the Roy Morgan poll gave them as historical examples are abnormally high, due to mass immigration, and atypical of normal (naturally established) populations. Few Australians, however, would realise how unusual Australia’s population growth rates have been.
Social desirability bias
Also, given how wanting lower immigration is stigmatised by the mass media and the government, which tend to conflate invited economic immigration with refugee or asylum-seeker migration, and protests about Muslim immigration as racist, it is likely that responses may have been affected by social desirability bias. Which would mean that this Roy Morgan poll would have been measuring what people have been taught is acceptable opinion rather than what they really think.
In an era of electronic surveillance, increased identity theft, phone scams and home invasion, how many people are likely to freely give an honest personal or political profile to some anonymous inquirer on the phone?
Although I also asked the Roy Morgan polsters a question about the use of randomized phone numbers, phone polls, the size of the group, and whether they used this same group size for their election polls, Roy Morgan did not get back to me.
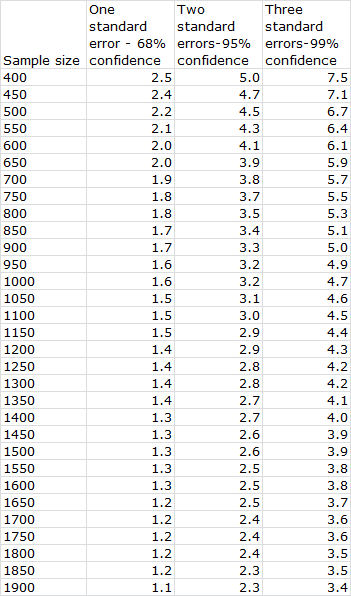
My understanding is that Roy Morgan polled a group of 650 people. This size group has a relatively high standard error.[5] The responses could be quite misleading.
The Roy Morgan polls were conducted by phone. A huge proportion of people select out of answering phone polls these days. As mentioned above, the response rate is something between 17 and 9 %. Although professional polling groups do studies on the huge and increasing refusal rate in phone polling, they usually conclude that this doesn’t make much difference. They base this conclusion on finding that small phone respondent groups have similar characteristics to larger groups of respondents to other methods, however the characteristics explored are not deep.
If survey groups revealed that their survey methods were very unreliable, they would go out of business. Think of your own reactions to phone surveys. In an era of electronic surveillance, increased identity theft, phone scams and home invasion, how many people are likely to freely give an honest personal or political profile to some anonymous inquirer on the phone?
Social desirability bias risks:
The responses the Morgan poll obtained were in accord with mainstream media propaganda which manufactures consent, rather than informs. The Australian mass-media and government consistently endorse high immigration and stigmatise as racist or ungenerous people who do not want high immigration. In polling there is a strong problem of social desirability bias, where people do not like to reveal to the polster that they hold views that vary from what perceived authorities deem desirable. This is particularly so on sensitised issues and the issue of immigration is strongly sensitised in Australia. In the Roy Morgan poll, the population growth question came after the survey group had been softened up by the immigration questions.
Misleading and vague
Although the survey informed people of approximately the numbers of [planned invited economic] permanent immigrants in 2014-2015, it did not mention the rate of temporary immigration nor the rate of conversion to permanent whilst in Australia, which comes to a much higher number. Nor did it mention that over 60 per cent of Australia's population growth comes from overseas immigration. There was no information about the recent high annual rate of growth of Australia’s population compared to that of other comparable OECD countries. Most people would not be able to tell you what that would mean in terms of doubling time anyway. Basically, there was no way for people to judge whether Australia’s population growth rate was normal or extreme. The survey questions lacked context and personal relevance.
What was the poll actually measuring?
The Roy Morgan poll did not establish that those surveyed actually knew the facts on what they were agreeing or disagreeing with. How valid were the responses in regards to population size and immigration? What did the poll actually measure? Impressions that immigration and population were 'under control' could be based on erroneous beliefs, such as that most immigrants are refugees, 'boat people' or asylum seekers; that the government has reduced this inflow, leading to the erroneous conclusion that Australia is getting hardly any immigrants and that the population may not be growing much at all from overseas immigration. Although you would think that people could work the situation out by looking at the growing traffic congestion, the fact is that, if asked a question about population or immigration without any prompting about congestion or housing shortages, for instance, most people do not make that connection.
Australian Institute of Progress Survey into Australian Community Attitudes to Immigration
The Australian Institute of Progress Australian Attitudes to Immigration reported that 69 per cent of its respondents were in favour of current or higher levels of immigration versus 27% who wanted less than current levels. (Table 1). But the institute admitted that
"Our percentages are not necessarily representative of the wider community with the same question in a poll commissioned by the Q Society finding 40.8 per cent thought that it was good. This is a significant discrepancy that we cannot explain." AIS, p. 6.
The Australian Institute for Progress's poll of 1349 respondents, from a non-random survey, gave similar results to the randomized Roy Morgan one, but it also asked questions which showed that a large proportion of those surveyed who agreed with higher immigration intake probably thought that most immigrants were refugees or asylum seekers, and may well have believed their numbers were less than 20,000 per annum, unaware of the far greater numbers of planned invited economic permanent immigrants, numbering around 250-300,000 per annum, or of short term immigrants.
The AIP Australian Attitudes to Immigration poll asked people for comments about the reasoning behind some of their answers and threw up plenty of misunderstandings indicating poor information about numbers and kinds of immigration to Australia. Few people seemed to understand that immigration increased population numbers and that this would affect their lives:
"The refugee issue affects what comes to mind when people talk about immigration. They often seem unaware that Australia is running a substantial non-refugee immigration program amounting to hundreds of thousands a year." (p.8.) "Many of those favouring an increase in immigration think that Australia takes far fewer immigrants than most other countries. (This is objectively wrong as can be seen in a comparison of net migration for all countries complied in the CIA factbook and available at "https://www.cia.gov/library/publications/the-world-factbook/rankorder/2112rank.html). (p.8.) [...] "Many of the respondents conflate immigration with the refugee issue." (p.12).
People opposed to immigration seemed to understand more about its role in population growth and how this would affect their lives:
"Those who are opposed to immigration are most likely to cite stress on infrastructure, housing, or the employment market." Australian Attitudes to Immigration, (p.10).
The Australian Institute of Progress does not claim that its results were for an average of Australians. Graham Young, Executive Director of the Australian Institute of Progress Poll told me in an email,
"[...] the survey sample has grown organically over the years. We picked-up a lot of respondents from the Australian newspaper at one stage. The ABC audience has also been a heavy contributor, and various parties have probably tried stacking it over the years. When I’ve done surveys of their media usage most don’t appear to use OLO. The largest single group of respondents seem to be Greens [...] [...] We did use other quantitative surveys as controls to ensure we weren’t too far out of whack." [6]
Mr Young sent me a report about the Morgan poll, suggesting that its similar results bore out the reliability of the Australian Institute of Progress poll. I would have thought the opposite, however, because, if the Morgan poll was adequately randomized and numerous as it claims, it should not agree with the Australian Institute of Progress poll, which surveyed a population probably dominated by refugee-focused Greens, with a dash of right-wingers from The Australian, some ABC viewers and lacking working class people.
Young compared the Australian Institute of Progress Poll to the much wider based 2013 Australian Electoral Study (mentioned near beginning of this article) which does include the ‘working class’ which last year showed very different results from the AIP ones. (See graph at beginning of this article.) The Electoral Study results were that only 24% favoured an increase in immigration, while 41% favoured a decrease and 35% favoured no change.[7] The 2013 Australian Electoral Study also posed its questions as abstract concepts.
For a quite different picture from those provided by Roy Morgan and the AIP, read about the prompted perception of impacts of population growth in South East Queensland, 2010 survey by Queensland Government. There are many reasons to argue that the Queensland survey method was an order of magnitude more valid than the other polls discussed above.
NOTES
[1] From the 2013 survey at http://ada.edu.au/ADAData/questionnaires/ADA.QUESTIONNAIRE.01259.pdf
"Completing the survey
This survey should take around half an hour to complete and your participation is entirely voluntary. If
you choose to participate, you can complete online by going to www.srcentre.com.au/aes and follow the
links. To access this survey you will need the username and password located in the panel in the top
right hand corner of this page. Alternatively, you can complete and return this questionnaire in the reply-
paid envelope provided. Respondents who complete the Australian Election Study early and return the
questionnaire by 26 September 2013 will be entered into a prize draw to win $500 cash. In total 3 x $500
will be drawn. For those who complete and return the questionnaire by 25 October 2013 you will also be
entered into a prize draw to win $500 cash (refer to prize draw terms and conditions of entry at
www.srcentre.com.au/aes). To assist you there are some instructions before the beginning of the
questionnaire about how to fill it out. Remember, it is important that we get your personal views on the
issues outlined in the questionnaire as well as some general information about yourself.
Confidentiality
Your views will remain strictly confidential and will be reported only as part of the general findings from
the survey. The only identifying feature on the questionnaire is a barcode which is used to avoid sending
you reminders after you have returned the completed questionnaire. The link between this barcode and
your name and address is securely stored and is destroyed once the survey is completed."
[2] Saskia Edwards, "Australians deeply divided on immigration policy," 13 October 2015 and "Australia divided on migration issues", The Australian, 13 October 2015.
[3] “Today 57% (up 22% since July 2010) of Australians support an Australian population of over 30 million in 30 years’ time – a stunning increase from only five years ago. Only 9% (down 15%) support a population of under 25 million, a further 23% (down 9%) support a population of 25-30 million and 11% (up 2%) can’t say.
A clear majority of Australians 69% (up 11%) support immigration (of 210,000 in 2013/14) remaining the same 37% (down 10%) or increasing 32% (up 21%) while 26% (down 14%) want immigration levels reduced and 5% (up 3%) can’t say.
Importantly, more Australians believe immigration has a positive effect on Australia 37% (up 4%) than a negative effect 31% (up 1%) while 19% (down 2%) believe immigration has little effect and 13% (down 3%) can’t say according to a special Morgan Poll conducted over three nights last week with a cross-section of 647 Australians aged 14+.
Not surprisingly, a vast majority of Australians support both Skilled migrant immigration (89% cf. 8% oppose) and Family reunion migration (79% cf. 16% oppose).
In addition, the negative debate about Muslims and Asylum seekers has had little impact on how Australians consider these types of migration – 65% of Australians support Muslim immigration up from 54% support in July 2010, while 28% of Australians oppose Muslim immigration.
A large majority of Australians support Asylum seeker immigration (71% up from 52% support in July 2010) while 21% of Australians oppose Asylum immigration.”
[4] For a sample size of 650 people, one standard error would be 2.0; two standard errors would be 3.9 and three standard errors would be 5.9.
To calculate the standard error take the square root of the following sum: the proportion you are interested in multiplied by the proportion of all the rest divided by the sample size.
The smaller the 'standard error', the more reliable the measure. Multiplying by 2 and 3 to get two and three etc standard errors is based on a theoretical second and third sample, and applies some kind of standard deviation norm which gives you the reliability.
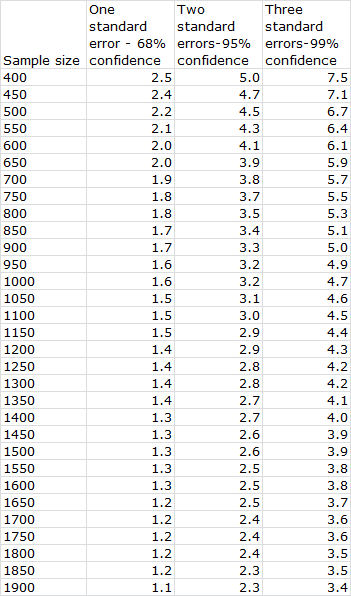
Reference: D. A. de Vaus, Surveys in Social Research, Allen and Unwin, Sydney, Allen and Unwin, 1995, pp. 151-2.
[5]
"[...] the survey sample has grown organically over the years. We picked-up a lot of respondents from the Australian newspaper at one stage. The ABC audience has also been a heavy contributor, and various parties have probably tried stacking it over the years. When I’ve done surveys of their media usage most don’t appear to use OLO. The largest single group of respondents seem to be Greens [...] [...] We did use other quantitative surveys as controls to ensure we weren’t too far out of whack." (Source: Email from Graham Young dated Sat, Oct 17, 2015 at 11:56 AM.)
[6] “Our respondents are likely to be more strongly in favour of continued migration than the bulk of the population, as the 2013 Australian Electoral Study shows 59% favouring current levels or higher, and 42% favouring lower levels. This probably reflects the fact that our surveys miss working class Australians. (Table 1).” Source: http://aip.asn.au/wp-content/uploads/2015/10/151013-AIP-Australian-Attitudes-to-Immigration-Report-FINAL.pdf, p.5.
[7] Here are the questions from the 2013 Australian Electoral Study that contain some relevance to population polls. You can download a copy of the study from: http://politicsir.cass.anu.edu.au/research/projects/electoral-surveys/australian-election-study/aes-2013
- Here is a list of important issues that were discussed during the election campaign. When you were deciding about how to vote, how important was each of these issues to you personally?
Issues Extremely important Quite important Not very important
1. Taxation ............................................ 1 2 3
2. Immigration ....................................... 1 2 3
3. Education .......................................... 1 2 3
4. The environment ............................... 1 2 3
5. Industrial relations ............................. 1 2 3
6. Health and Medicare ......................... 1 2 3
7. Refugees and asylum seekers .......... 1 2 3
8. Global warming ................................. 1 2 3
9. The carbon tax .................................. 1 2 3
10. Management of the economy ........... 1 2 3
- Still thinking about these same issues, whose policies—the Labor Party’s or the Liberal–National Coalition’s—would you say come closer to your own views on each of these issues?
- Still thinking about the same 10 issues, which of these issues was most important to you and your family during the election campaign? And which next?
Please put the number of the issue in the appropriate box below
Issue of most concern .............. Second issue of concern .............
- What do you think is the best way to handle the processing and resettlement of asylum seekers who come by boat and manage to reach Australian waters?
Process and resettle offshore .................................................................... 1
Process offshore but resettle in Australia .................................................. 2
Process and resettle onshore in Australia ................................................. 3
None of these options ................................................................................ 4
- Here are some statements about general social concerns. Please say whether you strongly agree, agree, disagree or strongly disagree with each of these statements.
The death penalty should be reintroduced for murder .....
The smoking of marijuana should NOT be a criminal offence
People who break the law should be given stiffer sentences
Women should be given preferential treatment when applying for jobs and promotions
All boats carrying asylum seekers should be turned back
Same-sex marriages should be prohibited by law
White Australians are advantaged over others in applying for jobs
It’s a problem if people think of themselves mostly as members of ethnic groups rather than as individuals.
The government should increase opportunities for women in business and industry
- Do you think the number of immigrants allowed into Australia nowadays should be reduced or increased?
Increased a lot ........................................................................................... 1
Increased a little ......................................................................................... 2
Remain about the same as it is ................................................................. 3
Reduced a little .......................................................................................... 4
Reduced a lot ............................................................................................. 5
- There are different opinions about the effects that immigrants have on Australia. How much do you agree or disagree with each of the following statements?
Strongly agree Agree Neither agree nor disagree Disagree Strongly disagree
Immigrants increase the crime rate ..... 1 2 3 4 5
Immigrants are generally good for Australia's economy ............................ 1 2 3 4 5
Immigrants take jobs away from people who are born in Australia ........ 1 2 3 4 5
Immigrants make Australia more open to new ideas and cultures .......... 1 2 3 4 5

 Australian freedom fighter and political refugee, Julian Assange, will take part in a discussion dedicated to information privacy and security in the digital age, organized as part of an RT conference on media and politics.
Australian freedom fighter and political refugee, Julian Assange, will take part in a discussion dedicated to information privacy and security in the digital age, organized as part of an RT conference on media and politics. 
 “Avoid culling roos for development by planning wildlife corridors,” says Craig Thomson, AWPC’s new Wildlife Planning Officer. In the face of state planning avoidance of obligation towards wildlife, Mr Thomson and AWPC want to crowdfund the purchase of private land to preserve wildlife corridors from being fenced off by farmers or built over by suburbia. The situation is increasingly dire for kangaroos and koalas particularly. Please consider helping this initiative. Contact details at end of article.
“Avoid culling roos for development by planning wildlife corridors,” says Craig Thomson, AWPC’s new Wildlife Planning Officer. In the face of state planning avoidance of obligation towards wildlife, Mr Thomson and AWPC want to crowdfund the purchase of private land to preserve wildlife corridors from being fenced off by farmers or built over by suburbia. The situation is increasingly dire for kangaroos and koalas particularly. Please consider helping this initiative. Contact details at end of article. On Monday 7 December 2015, the Australian Wildlife Protection Council (AWPC) announced its appointment of Mr Craig Thomson, of Wildlife Ecosystems Retention and Restoration, as their Wildlife Planning Officer.
On Monday 7 December 2015, the Australian Wildlife Protection Council (AWPC) announced its appointment of Mr Craig Thomson, of Wildlife Ecosystems Retention and Restoration, as their Wildlife Planning Officer. Video and transcript inside. Second in series.
Video and transcript inside. Second in series.  Sustainable Population Party finishes ahead of every other minor party in North Sydney by-election.
Sustainable Population Party finishes ahead of every other minor party in North Sydney by-election. Bruce Petty is a highly regarded political satirist and cartoonist as well as an award-winning film maker. He went to Syria in 2009 (before the war) on a project to interview Syrian intellectuals and university students about their political views. Dr Jeremy Salt is a former journalist, turned academic and is the author of The Unmaking of the Middle East. A History of Western Disorder in Arab Lands, (University of California Press, 2008). Until recently, Dr Salt was based in the Department of Political Science and Public Administration, Bilkent University, Ankara, Turkey, where he ran courses in the history of the modern Middle East, in politics and in politics, propaganda and the media. The story behind this series: On 16 November 2015 a small group of concerned Australian citizens got together to talk about the problems of getting real information out to Australians and other US-NATO allies about war in Syria, in spite of mainstream press efforts to confuse the public. Bruce Petty and Jeremy Salt were part of that group. Inside is the transcript of the embedded video. (There are two other videos in this series:
Bruce Petty is a highly regarded political satirist and cartoonist as well as an award-winning film maker. He went to Syria in 2009 (before the war) on a project to interview Syrian intellectuals and university students about their political views. Dr Jeremy Salt is a former journalist, turned academic and is the author of The Unmaking of the Middle East. A History of Western Disorder in Arab Lands, (University of California Press, 2008). Until recently, Dr Salt was based in the Department of Political Science and Public Administration, Bilkent University, Ankara, Turkey, where he ran courses in the history of the modern Middle East, in politics and in politics, propaganda and the media. The story behind this series: On 16 November 2015 a small group of concerned Australian citizens got together to talk about the problems of getting real information out to Australians and other US-NATO allies about war in Syria, in spite of mainstream press efforts to confuse the public. Bruce Petty and Jeremy Salt were part of that group. Inside is the transcript of the embedded video. (There are two other videos in this series:  This Queensland Survey demonstrates how superficial questioning about population growth as an abstract good or ill gives a completely different response from deeper, prompted questioning on the matter of experienced impact of population growth. Deeper questioning elicits a profound rejection of population growth and the colourful graphs reflect the real trends. We publish this analysis because of the counterintuitive results of two much publicised recent Victorian polls, by Roy Morgan and by the Australian Institute of Progress. Those poll results and methods are analysed in another article,
This Queensland Survey demonstrates how superficial questioning about population growth as an abstract good or ill gives a completely different response from deeper, prompted questioning on the matter of experienced impact of population growth. Deeper questioning elicits a profound rejection of population growth and the colourful graphs reflect the real trends. We publish this analysis because of the counterintuitive results of two much publicised recent Victorian polls, by Roy Morgan and by the Australian Institute of Progress. Those poll results and methods are analysed in another article, 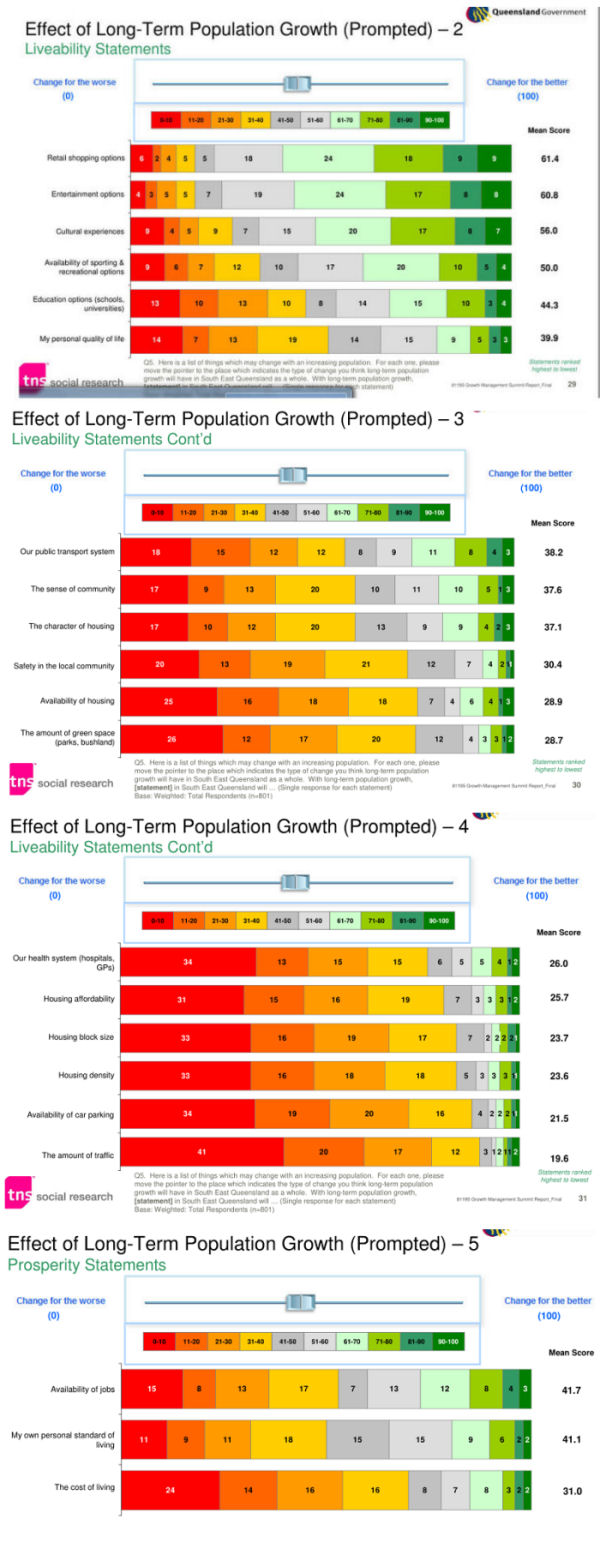
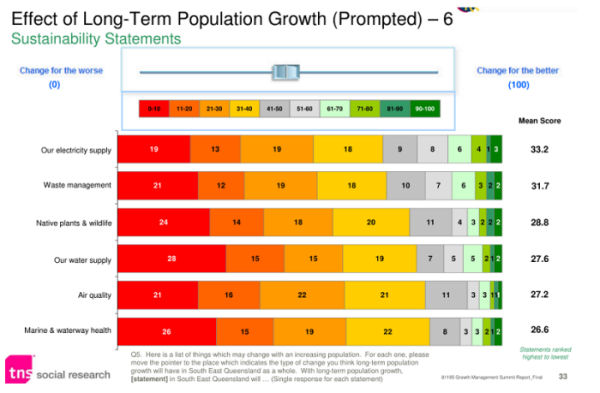
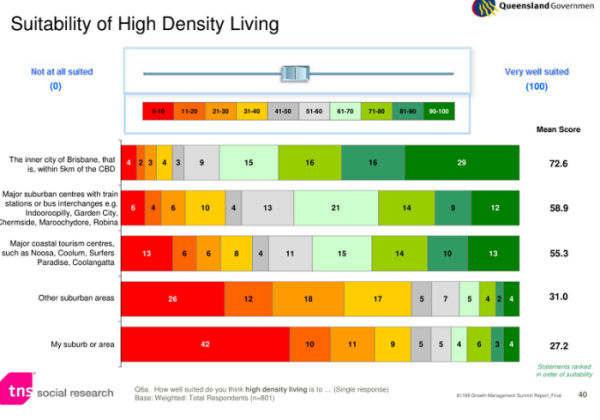 Prompted perception of impacts of population growth in South East Queensland, 2010 survey by Queensland Government
Prompted perception of impacts of population growth in South East Queensland, 2010 survey by Queensland Government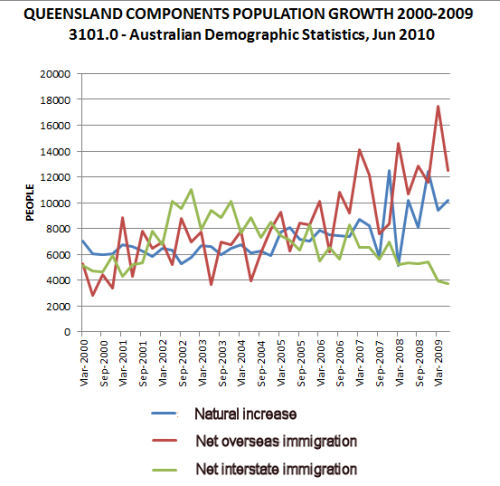
 What gives with surveys that tell us that most of us want more immigrants and a bigger population when, all around us, we suffer the effects of faster and faster population growth in groaning infrastructure, costly housing, road congestion, and rising costs for power and water? If we examine such studies, we will find that they pose their questions in the abstract and do not prompt people to make concrete associations about the effects of immigration and population growth. This is a bit like asking people how they feel about war compared to asking how they feel about war in their suburb. These polls also focus on ethnicity of immigrants rather than environment and planning impacts of mass migration. This article looks at recent polls by the
What gives with surveys that tell us that most of us want more immigrants and a bigger population when, all around us, we suffer the effects of faster and faster population growth in groaning infrastructure, costly housing, road congestion, and rising costs for power and water? If we examine such studies, we will find that they pose their questions in the abstract and do not prompt people to make concrete associations about the effects of immigration and population growth. This is a bit like asking people how they feel about war compared to asking how they feel about war in their suburb. These polls also focus on ethnicity of immigrants rather than environment and planning impacts of mass migration. This article looks at recent polls by the 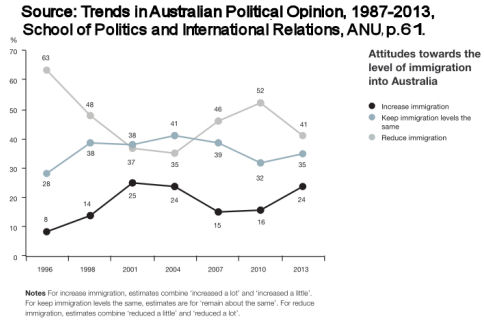
 If the downing of a Russian airliner in Sinai was in fact an act of terrorism, Western media's veritable gloating over the murder of tourists is another mark on their long record of shame. (Article first published in
If the downing of a Russian airliner in Sinai was in fact an act of terrorism, Western media's veritable gloating over the murder of tourists is another mark on their long record of shame. (Article first published in 
 We are a small group of Yarra River users : walkers, cyclists and rowers, and we are absolutely appalled by a proposed new apartment development by Salta on the Yarra Riverbank in Abbotsford. The developer is submitting in the busy period before Christmas, and before more onerous planning controls apply in 2016.
We are a small group of Yarra River users : walkers, cyclists and rowers, and we are absolutely appalled by a proposed new apartment development by Salta on the Yarra Riverbank in Abbotsford. The developer is submitting in the busy period before Christmas, and before more onerous planning controls apply in 2016.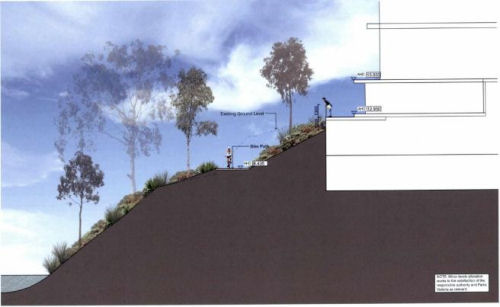 The cycle/pedestrian path is right beside the enormous building, and on the plans the proposal lowers the PUBLIC path to accommodate the development. If it is approved, the path is likely to be closed for as long as the development takes to build. If built, recreational users will have vastly lessened amenity and access to green space and open space. A canyon like effect will be created which will completely overwhelm and destroy the pleasant and tranquil surroundings.
The cycle/pedestrian path is right beside the enormous building, and on the plans the proposal lowers the PUBLIC path to accommodate the development. If it is approved, the path is likely to be closed for as long as the development takes to build. If built, recreational users will have vastly lessened amenity and access to green space and open space. A canyon like effect will be created which will completely overwhelm and destroy the pleasant and tranquil surroundings. video inside:In a huge stunning announcement yesterday by the Russian Foreign Minister, Russia presented direct evidence of Turkey buying illegal oil from the black market supporting terrorists. In this video change.org goes over the important revelations by the Russians, their consequences and the shift of the geopolitical field. The western mainstream media is simply not reporting this because it runs totally counter to their spin. If the western media were to properly bring this news to their readers, they would have to explain the torrent of lies they have issued forth so far in order to justify war. The western media is historically pro-war and Australians, Americans, British and Europeans who rely on the mainstream media alone never hear both sides.
video inside:In a huge stunning announcement yesterday by the Russian Foreign Minister, Russia presented direct evidence of Turkey buying illegal oil from the black market supporting terrorists. In this video change.org goes over the important revelations by the Russians, their consequences and the shift of the geopolitical field. The western mainstream media is simply not reporting this because it runs totally counter to their spin. If the western media were to properly bring this news to their readers, they would have to explain the torrent of lies they have issued forth so far in order to justify war. The western media is historically pro-war and Australians, Americans, British and Europeans who rely on the mainstream media alone never hear both sides. Following the ISIS outrages in Beirut and Paris, John Pilger updates this prescient essay on the root causes of terrorism and what we can do about it. In transmitting President Richard Nixon's orders for a "massive" bombing of Cambodia in 1969, Henry Kissinger said, "Anything that flies on everything that moves". As Barack Obama wages his seventh war against the Muslim world since he was awarded the Nobel Peace Prize, and Francois Hollande promises a "merciless" attack on the rubble of Syria, the orchestrated hysteria and lies make one almost nostalgic for Kissinger's murderous honesty.
Following the ISIS outrages in Beirut and Paris, John Pilger updates this prescient essay on the root causes of terrorism and what we can do about it. In transmitting President Richard Nixon's orders for a "massive" bombing of Cambodia in 1969, Henry Kissinger said, "Anything that flies on everything that moves". As Barack Obama wages his seventh war against the Muslim world since he was awarded the Nobel Peace Prize, and Francois Hollande promises a "merciless" attack on the rubble of Syria, the orchestrated hysteria and lies make one almost nostalgic for Kissinger's murderous honesty.
 Video inside:One of NATO imperialism's greatest chroniclers, Australian award-winning journalist and filmmaker, John Pilger, tells us how Washington, London and Paris gave birth to ISIS.
Video inside:One of NATO imperialism's greatest chroniclers, Australian award-winning journalist and filmmaker, John Pilger, tells us how Washington, London and Paris gave birth to ISIS. Update: See new article,
Update: See new article, 

 On Thursday the fifth of November 2015, local, state and federal representatives from The Greens launched their plan for a “Better More Liveable Melbourne” but what impact will this plan have considering Victoria's population is increasing by a hundred thousand a year (especially when most of the growth is in Melbourne)?
On Thursday the fifth of November 2015, local, state and federal representatives from The Greens launched their plan for a “Better More Liveable Melbourne” but what impact will this plan have considering Victoria's population is increasing by a hundred thousand a year (especially when most of the growth is in Melbourne)? At first glance it appears that it would have a major impact, especially as the aim of the plan is to invest heavily in a wide range of projects including three new railway stations, schools in the Docklands, fifty new trams running on 100% renewable energy, a railway line to Doncaster and an upgrade of the train signalling system.
At first glance it appears that it would have a major impact, especially as the aim of the plan is to invest heavily in a wide range of projects including three new railway stations, schools in the Docklands, fifty new trams running on 100% renewable energy, a railway line to Doncaster and an upgrade of the train signalling system. 


 Australian comedian Barry Humphries' humour identified and targeted a world of pleasant streets and gardens that is now under threat. We've stopped laughing, but is it too late?
Australian comedian Barry Humphries' humour identified and targeted a world of pleasant streets and gardens that is now under threat. We've stopped laughing, but is it too late?


 One dramatic impact of the Paris terror attack and the contradictions within the NATO camp and vis a vis the GCC-Turkish Camp, is that all of Putin's worst detractors are queuing up to meet him and seek his words of wisdom ....
One dramatic impact of the Paris terror attack and the contradictions within the NATO camp and vis a vis the GCC-Turkish Camp, is that all of Putin's worst detractors are queuing up to meet him and seek his words of wisdom .... The photos of Putin, Obama with their 2 advisors sitting around a table for just 4 has gone all across the world
The photos of Putin, Obama with their 2 advisors sitting around a table for just 4 has gone all across the world
 This happened last night:
This happened last night:  Cartoon of the day by
Cartoon of the day by 


 The Middle East conflict - war in Syria and Iraq - has already spilled over. No one is safe from the terrorist attacks, neither East, nor West. Islamic State claims it is still strong, and its ideas are attracting new recruits to replace those killed on the field. Islamic State says the horrors it perpetrates are done in the name Allah - spurring resentment against Muslims all across the globe. Today, we speak to an Islamic scholar, a Grand Mufti of Syria, Ahmad Badreddin Hassoun, to see how the jihadists have twisted the idea of Islam. And does their agenda have anything to do with Islam at all? Republished from
The Middle East conflict - war in Syria and Iraq - has already spilled over. No one is safe from the terrorist attacks, neither East, nor West. Islamic State claims it is still strong, and its ideas are attracting new recruits to replace those killed on the field. Islamic State says the horrors it perpetrates are done in the name Allah - spurring resentment against Muslims all across the globe. Today, we speak to an Islamic scholar, a Grand Mufti of Syria, Ahmad Badreddin Hassoun, to see how the jihadists have twisted the idea of Islam. And does their agenda have anything to do with Islam at all? Republished from 


 Review of Kenneth Eade's The Involuntary Spy: Who among us realised that Monsanto has huge plans for Ukraine? We learn that Ukraine's current president, Poreschenko, has been in cahoots with the US for years, and that Monsanto has been buying up land and lobbying to change Ukraine's anti-GMO laws, inserting a key clause in an EU Association agreement.
Review of Kenneth Eade's The Involuntary Spy: Who among us realised that Monsanto has huge plans for Ukraine? We learn that Ukraine's current president, Poreschenko, has been in cahoots with the US for years, and that Monsanto has been buying up land and lobbying to change Ukraine's anti-GMO laws, inserting a key clause in an EU Association agreement.
 Venue: Mulgrave Country Club, Saturday 14 November, 9.30am to 4pm. Join us and other ratepayer leaders to discuss about common core issues and how the LG Act and other associated laws, and the roles of ratepayer groups can be changed to fix today’s broken LG system for the better. The seminar will include free light lunch and feature inspirational speakers.
Venue: Mulgrave Country Club, Saturday 14 November, 9.30am to 4pm. Join us and other ratepayer leaders to discuss about common core issues and how the LG Act and other associated laws, and the roles of ratepayer groups can be changed to fix today’s broken LG system for the better. The seminar will include free light lunch and feature inspirational speakers.


 If you have a heart please don't ignore this post - we need to let the whole world know what's happening. Boycott palm oil products now. Please donate to the campaign. Because of forest clearing for palm oil, in just the last 20 years 90% of orangutan habitat has already been destroyed. If deforestation continues at this pace, orangutans could be extinct in the wild as early as 2015, and their jungle habitat could be completely gone in 20 years from now. Donate at
If you have a heart please don't ignore this post - we need to let the whole world know what's happening. Boycott palm oil products now. Please donate to the campaign. Because of forest clearing for palm oil, in just the last 20 years 90% of orangutan habitat has already been destroyed. If deforestation continues at this pace, orangutans could be extinct in the wild as early as 2015, and their jungle habitat could be completely gone in 20 years from now. Donate at 


 Confused about what the US and NATO are doing about Syria? Not satisfied with explanations in the mainstream press? Worried that we are promoting more refugees instead of peace in the region? This article gives a very good simple overview of the history and society in Syria, regional religious pressures, recent events and politics, including water theft, background to ISIS, and Turkey's role in opening the refugee floodgates towards Europe. This article represents the text of a talk at a panel on Syrian refugees given by the author in the United States. You can read more of Judy's work on
Confused about what the US and NATO are doing about Syria? Not satisfied with explanations in the mainstream press? Worried that we are promoting more refugees instead of peace in the region? This article gives a very good simple overview of the history and society in Syria, regional religious pressures, recent events and politics, including water theft, background to ISIS, and Turkey's role in opening the refugee floodgates towards Europe. This article represents the text of a talk at a panel on Syrian refugees given by the author in the United States. You can read more of Judy's work on 


 A logger recently posted this nasty message to forest activists on a day when they were meeting to negotiate the protection of giant trees.
A logger recently posted this nasty message to forest activists on a day when they were meeting to negotiate the protection of giant trees.
 ALEPPO, SYRIA: Since the Russians began helping the Syrian Arab Army to drive ISIS out, a jealous United States, furious that its goal of destroying Syria might yet fail, has spitefully disseminated unconfirmed stories aimed at discrediting Russia's motives and performance. The latest by British Airforce doctor, David Nott, who has also been associated with the charity Syria Relief, alleges that Russia has been purposefully destroying hospitals in Syria.[1] This is ironic when the US itself was so recently caught out bombing a Doctors without Borders manned-hospital in Afghanistan in what almost no-one denies was a blatant war crime.[2] In Syria, the roads supplying food and fuel to Aleppo have only just been reconnected since being cut off by ISIS a few days ago, in attacks that appear to have been facilitated by the US. But ISIS continues to be refueled with fighters who come in via Australia's ally, Turkey, where Muslim Brotherhood supporter, President Erdogan, is seeking to change the laws to make himself a full dictator. Our correspondent in Aleppo, Syria, vents his disgust at these beat-ups.
ALEPPO, SYRIA: Since the Russians began helping the Syrian Arab Army to drive ISIS out, a jealous United States, furious that its goal of destroying Syria might yet fail, has spitefully disseminated unconfirmed stories aimed at discrediting Russia's motives and performance. The latest by British Airforce doctor, David Nott, who has also been associated with the charity Syria Relief, alleges that Russia has been purposefully destroying hospitals in Syria.[1] This is ironic when the US itself was so recently caught out bombing a Doctors without Borders manned-hospital in Afghanistan in what almost no-one denies was a blatant war crime.[2] In Syria, the roads supplying food and fuel to Aleppo have only just been reconnected since being cut off by ISIS a few days ago, in attacks that appear to have been facilitated by the US. But ISIS continues to be refueled with fighters who come in via Australia's ally, Turkey, where Muslim Brotherhood supporter, President Erdogan, is seeking to change the laws to make himself a full dictator. Our correspondent in Aleppo, Syria, vents his disgust at these beat-ups.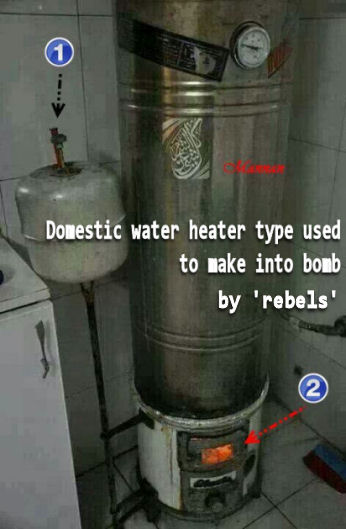
 The following letter from the Australian Wildlife Protection Council Inc. to the Victorian Ombudsman urgently signals the failure of Victorian law to protect Victorian wildlife and the lack of standing for wildlife carers against ill-based and frequent cull permits to farmers in a situation where no-one actually counts the kangaroos or actual ferals, like rabbits. The situation is truly scandalous; Victoria's almost useless laws were conceived and are administered with utter cynicism.
The following letter from the Australian Wildlife Protection Council Inc. to the Victorian Ombudsman urgently signals the failure of Victorian law to protect Victorian wildlife and the lack of standing for wildlife carers against ill-based and frequent cull permits to farmers in a situation where no-one actually counts the kangaroos or actual ferals, like rabbits. The situation is truly scandalous; Victoria's almost useless laws were conceived and are administered with utter cynicism.
 Do you remember the last time you saw a man with wild eyes, strange clothes and a giant sign around his neck saying “The End Is Nigh”? “How ridiculous and pathetic!” you might have thought. Now, imagine the reality of your country changing within weeks to a point where you come to the same conclusion as him, suddenly feeling that his approach might be ever so reasonable. When a large part of your fellow-humans catch a strange sort of illness, one which leads to complete insanity faster than in the worst zombie outbreak, you might find yourself out of more viable strategies.
Do you remember the last time you saw a man with wild eyes, strange clothes and a giant sign around his neck saying “The End Is Nigh”? “How ridiculous and pathetic!” you might have thought. Now, imagine the reality of your country changing within weeks to a point where you come to the same conclusion as him, suddenly feeling that his approach might be ever so reasonable. When a large part of your fellow-humans catch a strange sort of illness, one which leads to complete insanity faster than in the worst zombie outbreak, you might find yourself out of more viable strategies.
Recent comments